Blog
Age-related macular degeneration, often called ARMD or AMD, is the leading cause of vision loss among Americans 65 and older.
AMD causes damage to the macula, which is the central portion of the retina responsible for sharp central vision. AMD doesn't lead to complete blindness because peripheral vision is still intact, but the loss of central vision can interfere with simple everyday activities such as reading and driving, and it can be debilitating.
Types of Macular Degeneration
There are two types of macular degeneration: Dry AMD and Wet AMD.
Dry (non-exudative) macular degeneration constitutes approximately 85-90% of all cases of AMD. Dry AMD results from thinning of the macula or the deposition of yellow pigment known as drusen in the macula. There may be gradual loss of central vision with dry AMD, but it is usually not as severe as wet AMD vision loss. However, dry AMD can slowly progress to late-stage geographic atrophy, which can cause severe vision loss.
Wet (exudative) macular degeneration makes up the remaining 10-15% of cases. Exudative or neovascular refers to the growth of new blood vessels in the macula, where they are not normally present. The wet form usually leads to more serious vision loss than the dry form.
AMD Risk factors
- Age is the biggest risk factor. Risk increases with age.
- Smoking. Research shows that smoking increases your risk.
- Family history. People with a family history of AMD are at higher risk.
- Race. AMD is more common in Caucasians than other races, but it exists in every ethnicity.
- Light eyes. Blue and hazel eyes are more prone to AMD than brown eyes.
- Gender. AMD is more common in women than men.
- High blood pressure.
- Diet high in saturated fat.
Detection of AMD
There are several tests that are used to detect AMD.
A dilated eye exam can detect AMD. Once the eyes are dilated, the macula can be viewed by the ophthalmologist or optometrist. The presence of drusen and pigmentary changes can then be detected.
An Amsler Grid test uses pattern of straight lines that resemble a checkerboard. It can be used to monitor changes in vision. The onset of AMD can cause the lines on the grid to disappear or appear wavy and distorted.
Fluorescein Angiogram is a test performed in the office. A fluorescent dye is injected into the arm and then a series of pictures are taken as the dye passes through the circulatory system in the back of the eye.
Optical coherence tomography (OCT) is a test based on ultrasound. It is a painless study where high-resolution pictures are taken of the retina.
Article contributed by Jane Pan M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
For over 40 years the standard surgical treatment for glaucoma was a procedure called a trabeculectomy.
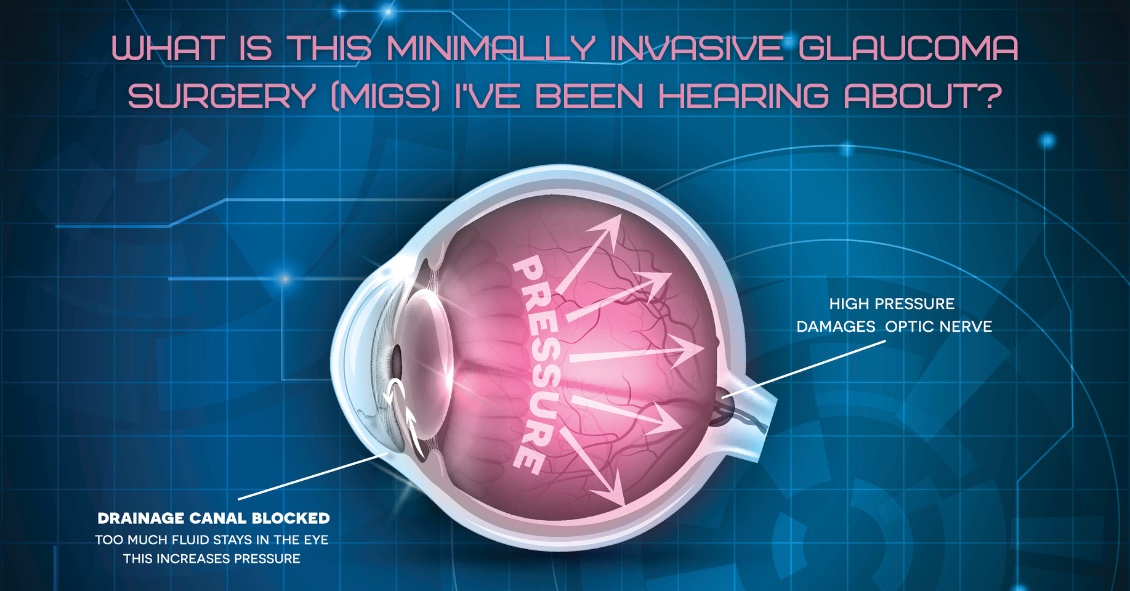
In a trabeculectomy, the ophthalmic surgeon would make a hole in the wall of eye to allow fluid from the inside of the eye to flow out of the eye and then get resorbed by the blood vessels in the conjunctiva (the mucous membrane that covers the white part of the eye).
This surgery often resulted in a large decrease in the Intraocular Pressure (IOP). Reducing the IOP is the goal of glaucoma surgery because multiple studies show that if you can reduce the pressure the progression of glaucoma slows.
The problem with trabeculectomy is that although it frequently lowers the pressure, it also has a fairly high complication and/or failure rate. This led to some reluctance to perform the procedure unless the glaucoma was severe, or the pressure was very high. As a result of those issues there has been a search during the last 40 years for something that had a lower complication rate and could be more easily deployed earlier in the disease process.
Enter Minimally Invasive Glaucoma Surgery, or MIGS. There are now several types of surgeries that fit in the MIGS category and many of them are used in conjunction with cataract surgery. They are utilized much earlier in the disease process and when combined with cataract surgery they can be used to not only help control the pressure over the long term but can often even reduce the burden of eye drops afterward.
The biggest advantage to MIGS over the trabeculectomy is that when used in conjunction with cataract surgery, MIGS can lower the eye pressure (although not as much as the trabeculectomy) but often with no higher rate of complications as there is with cataract surgery alone.
The lower complication rate is mainly because the MIGS procedures do not create a full-thickness hole in the wall of the eye. Most of them involve putting in some form of stent inside the eye. The stent lets the intraocular fluid get out of the eye more efficiently through its normal internal drain called the trabecular meshwork, rather than having to flow to the outside of the eye as with a trabeculectomy.
A stent is not the only way to lower the pressure along with cataract surgery. There is also a laser treatment you can do from the inside of the eye that slows the amount of fluid the eye makes, which also results in a lower pressure. It is called Endocyclophotocoagulation (ECP). Think of a partially clogged drain in a sink with constantly running water. If you don’t want the sink to overflow (or the pressure in the eye to get too high) you either try to unclog the drain (stent) or you turn down the faucet (ECP).
MIGS has been a great development over the last several years, enabling the surgeon to intervene at a much earlier stage of glaucoma and with a significantly lower complication rate than the more invasive trabeculectomy.
At this point I utilize one of the MIGS procedures in almost all patients who need their cataracts removed and are on one or more glaucoma medications. Even if the glaucoma is fairly well controlled at the time, the MIGS procedure gives us the opportunity to try and get a glaucoma patient off their eye drops, which is both a decreased burden of treatment and lets us keep the eye drops in reserve should the pressure start to increase again later in life.
If you have glaucoma and a cataract you should definitely discuss this with your doctor to see if a MIGS procedure along with your cataract surgery could be the right choice for you.
Article contributed by Dr. Brian Wnorowski, M.D.