Blog
Eye doctors typically pride themselves on being able to improve someone’s vision through glasses or contact lens prescriptions. Whether it’s a first-time glasses wearer, or someone having either a small or large change in their prescription, we like to aim for that goal of 20/20 vision.
Despite our best efforts, however, correcting vision to 20/20 is not always a positive outcome for the patient. Whether someone will be able to tolerate their new prescription is based on something called neuroplasticity, which is what allows our brains to adapt to changes in our vision.
You or someone you know may have had this happen: Your vision was blurry, so you went to the eye doctor. The doctor gave you a new prescription, but after you received your new glasses, things seem “off.”
Common complaints are that the prescription feels too strong (or even too clear!) or that the wearer feels dizzy or faint. This is especially true with older patients who have had large changes in their prescriptions, since neuroplasticity decreases with age. It is also more likely to happen when the new prescription has a change in the strength or the angle of astigmatism correction. Conversely, this happens less often in children, since their brains have a high amount of plasticity.
Quite often, giving the brain enough time to adapt to the new vision will decrease these symptoms.
Whenever a patient has a large change in prescription, I tell them that they should wear the glasses full time for at least one week. This is true for both large changes in prescription strength, as well as changing lens modality, e.g., single vision to progressives.
Despite the patient’s best efforts, though, sometimes allowing time to adapt to the new vision isn’t enough, and the prescription needs to be adjusted. Even when someone sees 20/20 on the eye chart with their new glasses, if they are uncomfortable in them even after trying to adjust for a week then we sometimes have to make a compromise and move the script back closer to their previous script so that there is less change and they can more easily adapt.
In conclusion, adapting to a new prescription can sometimes be frustrating. It does not mean there is anything wrong with you if you have difficulty adjusting to large changes in a prescription. With a little patience and understanding about how your brain adapts to these kinds of changes, your likelihood of success will be that much higher.
Article contributed by Dr. Jonathan Gerard
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
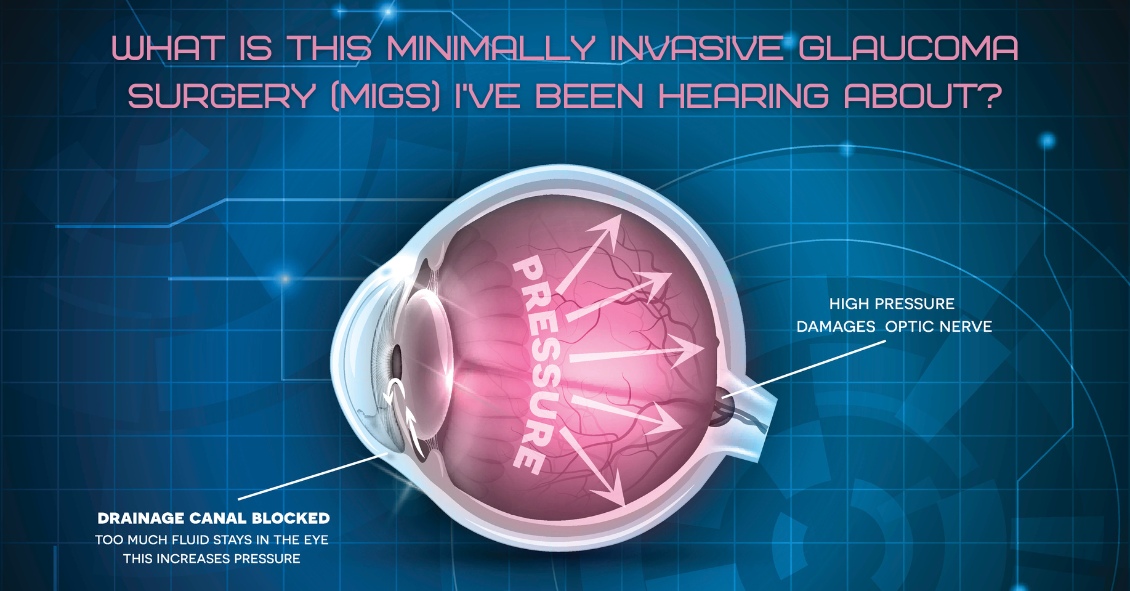
For over 40 years the standard surgical treatment for glaucoma was a procedure called a trabeculectomy.
In a trabeculectomy, the ophthalmic surgeon would make a hole in the wall of eye to allow fluid from the inside of the eye to flow out of the eye and then get resorbed by the blood vessels in the conjunctiva (the mucous membrane that covers the white part of the eye).
This surgery often resulted in a large decrease in the Intraocular Pressure (IOP). Reducing the IOP is the goal of glaucoma surgery because multiple studies show that if you can reduce the pressure the progression of glaucoma slows.
The problem with trabeculectomy is that although it frequently lowers the pressure, it also has a fairly high complication and/or failure rate. This led to some reluctance to perform the procedure unless the glaucoma was severe, or the pressure was very high. As a result of those issues there has been a search during the last 40 years for something that had a lower complication rate and could be more easily deployed earlier in the disease process.
Enter Minimally Invasive Glaucoma Surgery, or MIGS. There are now several types of surgeries that fit in the MIGS category and many of them are used in conjunction with cataract surgery. They are utilized much earlier in the disease process and when combined with cataract surgery they can be used to not only help control the pressure over the long term but can often even reduce the burden of eye drops afterward.
The biggest advantage to MIGS over the trabeculectomy is that when used in conjunction with cataract surgery, MIGS can lower the eye pressure (although not as much as the trabeculectomy) but often with no higher rate of complications as there is with cataract surgery alone.
The lower complication rate is mainly because the MIGS procedures do not create a full-thickness hole in the wall of the eye. Most of them involve putting in some form of stent inside the eye. The stent lets the intraocular fluid get out of the eye more efficiently through its normal internal drain called the trabecular meshwork, rather than having to flow to the outside of the eye as with a trabeculectomy.
A stent is not the only way to lower the pressure along with cataract surgery. There is also a laser treatment you can do from the inside of the eye that slows the amount of fluid the eye makes, which also results in a lower pressure. It is called Endocyclophotocoagulation (ECP). Think of a partially clogged drain in a sink with constantly running water. If you don’t want the sink to overflow (or the pressure in the eye to get too high) you either try to unclog the drain (stent) or you turn down the faucet (ECP).
MIGS has been a great development over the last several years, enabling the surgeon to intervene at a much earlier stage of glaucoma and with a significantly lower complication rate than the more invasive trabeculectomy.
At this point I utilize one of the MIGS procedures in almost all patients who need their cataracts removed and are on one or more glaucoma medications. Even if the glaucoma is fairly well controlled at the time, the MIGS procedure gives us the opportunity to try and get a glaucoma patient off their eye drops, which is both a decreased burden of treatment and lets us keep the eye drops in reserve should the pressure start to increase again later in life.
If you have glaucoma and a cataract you should definitely discuss this with your doctor to see if a MIGS procedure along with your cataract surgery could be the right choice for you.
Article contributed by Dr. Brian Wnorowski, M.D.